The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in the regulation of various bodily functions. Located in the brainstem, this long and complex nerve extends throughout the body, including the stomach. Cutting the vagus nerve to the stomach can have significant implications on an individual’s health and well-being.
Understanding the Vagus Nerve
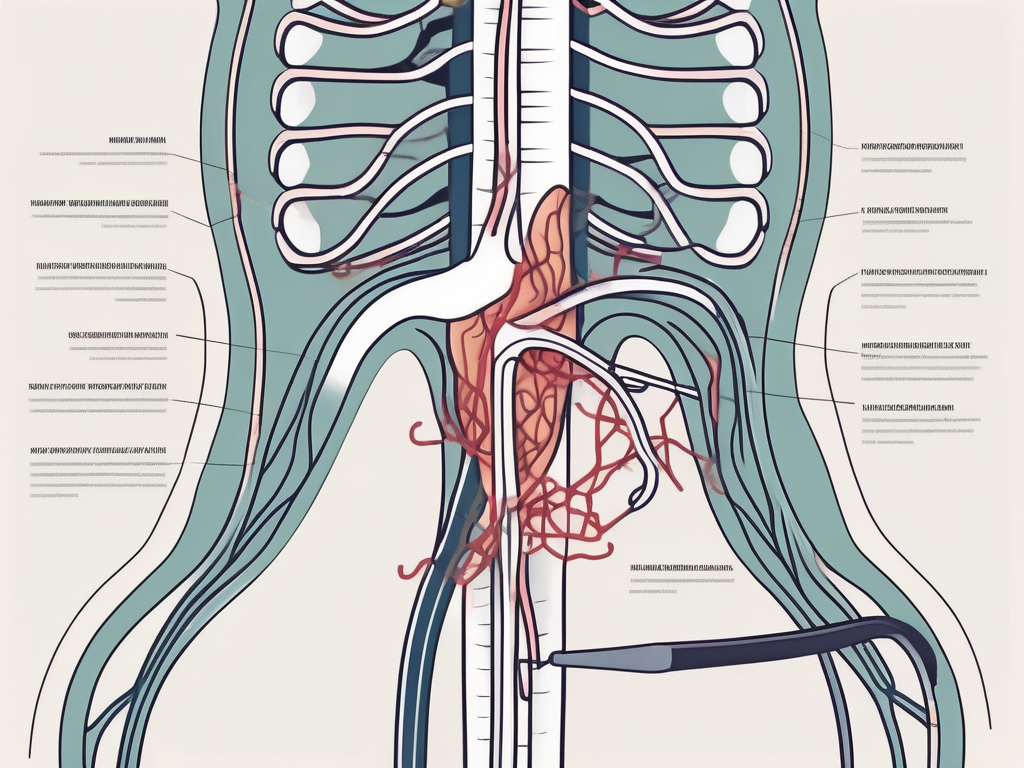
The vagus nerve, originating in the medulla oblongata, is responsible for the parasympathetic control of many vital bodily functions. It carries sensory information from the organs back to the brain and controls the autonomous processes such as heart rate, digestion, and breathing. Its intricate network of fibers reaches into various organs, including the stomach, making it an integral part of the body’s functioning.
The Role of the Vagus Nerve in the Body
The vagus nerve is often referred to as the “wandering nerve” due to its extensive reach throughout the body. It regulates digestion by stimulating the production of stomach acid and digestive enzymes, as well as managing the movement of food through the digestive tract. Additionally, it helps regulate heart rate, blood pressure, and breathing, contributing to overall homeostasis.
But the vagus nerve’s role goes beyond just digestion and basic bodily functions. Recent research has shown that it also plays a crucial role in the brain-gut axis, which is the bidirectional communication between the brain and the gut. This means that the vagus nerve not only receives signals from the brain to control digestion, but it also sends signals back to the brain, influencing mood, emotions, and even cognitive function.
Furthermore, the vagus nerve is involved in the body’s stress response. When we experience stress, the vagus nerve helps activate the parasympathetic nervous system, which promotes relaxation and helps counteract the effects of the sympathetic nervous system, responsible for the “fight or flight” response. This intricate interplay between the vagus nerve and the stress response highlights its importance in maintaining overall well-being.
The Vagus Nerve and the Stomach: A Crucial Connection
The connection between the vagus nerve and the stomach is crucial for proper digestion. When food enters the stomach, the vagus nerve sends signals to stimulate the release of gastric acid and enzymes required for effective digestion. It also controls the movement of muscles in the stomach, aiding in the breakdown and mixing of food to facilitate nutrient absorption.
But did you know that the vagus nerve’s influence on the stomach goes beyond digestion? Research has shown that the vagus nerve also plays a role in appetite regulation. It communicates with the brain to signal feelings of fullness and satiety, helping us know when to stop eating. This intricate feedback loop between the stomach and the vagus nerve ensures that we maintain a healthy balance of food intake.
In addition to its role in digestion and appetite regulation, the vagus nerve also influences the gut microbiome. The gut microbiome refers to the trillions of microorganisms that inhabit our digestive system and play a crucial role in our overall health. Studies have shown that the vagus nerve helps maintain a healthy balance of gut bacteria by regulating the production of antimicrobial peptides and promoting the growth of beneficial bacteria.
Overall, the vagus nerve’s connection to the stomach is not just limited to digestion. It encompasses a wide range of functions, from appetite regulation to gut microbiome maintenance, highlighting its significance in maintaining optimal health.
The Surgical Procedure: Cutting the Vagus Nerve
Cutting the vagus nerve to the stomach is a surgical procedure that should only be undertaken under specific circumstances and medical supervision. It involves severing the nerve, disrupting its communication with the stomach and interrupting its normal functioning.
Reasons for Cutting the Vagus Nerve
While cutting the vagus nerve is not a common medical procedure, it may be considered in certain situations, such as the treatment of severe cases of obesity or gastrointestinal disorders that have not responded to other treatments. Obesity, a complex condition characterized by excessive body fat accumulation, can have serious health consequences, including an increased risk of heart disease, diabetes, and certain types of cancer. In cases where other weight loss interventions have failed, cutting the vagus nerve may be an option to help reduce appetite and promote weight loss.
Gastrointestinal disorders, on the other hand, refer to a group of conditions that affect the digestive system, such as gastroparesis, a condition in which the stomach takes too long to empty its contents. When other treatments, such as dietary changes, medications, and lifestyle modifications, have not provided sufficient relief, cutting the vagus nerve may be considered as a last resort to alleviate symptoms and improve quality of life.
It is important to note that this decision is made on a case-by-case basis, after careful consideration of the potential risks and benefits. The patient’s overall health, medical history, and individual circumstances are taken into account to determine whether cutting the vagus nerve is the most appropriate course of action.
The Process of Vagus Nerve Cutting
The surgical process involves identifying the vagus nerve and carefully severing it. The vagus nerve, also known as the tenth cranial nerve, is a long and complex nerve that originates in the brainstem and extends down to various organs in the body, including the stomach. It plays a crucial role in regulating many bodily functions, including digestion, heart rate, and breathing.
Before the procedure, the patient is typically placed under general anesthesia to ensure their comfort and safety. Once the anesthesia has taken effect, the surgeon makes an incision in the abdomen to access the area where the vagus nerve is located. Specialized instruments and techniques are used to carefully identify and isolate the nerve.
Once the vagus nerve is visualized, the surgeon proceeds to carefully sever it. This step requires precision and expertise to minimize potential complications. The severed ends of the nerve are then either left as is or sometimes capped with a special material to prevent reconnection.
After the nerve is cut, its normal communication with the stomach is disrupted. This interruption can lead to changes in stomach function, such as reduced acid production and delayed emptying. These changes can have both positive and negative effects on the patient’s overall health and well-being, depending on the underlying condition being treated.
Following the procedure, the patient is closely monitored in a hospital setting to ensure proper healing and to manage any potential complications. The recovery period can vary depending on the individual and the specific circumstances of the surgery. Close follow-up with the healthcare team is essential to monitor the patient’s progress and address any concerns that may arise.
Potential Consequences of Cutting the Vagus Nerve
The consequences of cutting the vagus nerve to the stomach can have both immediate physical effects and long-term health implications. It is essential to understand these potential consequences before considering such a procedure.
The vagus nerve plays a crucial role in regulating various functions of the stomach. By transmitting signals between the brain and the stomach, it helps maintain a delicate balance in digestion and overall gastrointestinal health. However, cutting this nerve can disrupt this intricate system, leading to a cascade of effects on the body.
Immediate Physical Effects
Immediately after cutting the vagus nerve, individuals may experience a reduction in appetite due to the disruption of the nerve’s signaling to the brain. This can lead to weight loss. The brain, no longer receiving the usual signals of hunger and satiety, may struggle to regulate food intake effectively.
In addition to changes in appetite, some individuals may experience symptoms such as nausea, vomiting, and bloating. These discomforts arise as the normal regulation of stomach functions is compromised. Without the vagus nerve’s influence, the stomach may struggle to coordinate the release of digestive enzymes and the movement of food through the digestive tract.
Long-Term Health Implications
Long-term implications of cutting the vagus nerve can vary depending on the individual and the specific circumstances. Potential complications may include difficulties with digestion, including delayed emptying of the stomach, malabsorption of nutrients, and an increased risk of developing gastrointestinal disorders.
Delayed gastric emptying, also known as gastroparesis, is a common long-term consequence of cutting the vagus nerve. This condition occurs when the stomach takes longer than usual to empty its contents into the small intestine. As a result, individuals may experience symptoms such as bloating, abdominal pain, and a feeling of fullness even after consuming small amounts of food.
Malabsorption of nutrients is another concern that arises from cutting the vagus nerve. Without proper signaling from the nerve, the stomach may not release enough digestive enzymes and acids to break down food effectively. This can lead to inadequate absorption of essential nutrients, such as vitamins and minerals, potentially resulting in nutritional deficiencies.
Furthermore, the disruption of the vagus nerve’s function can increase the risk of developing gastrointestinal disorders. Conditions such as gastroesophageal reflux disease (GERD), peptic ulcers, and irritable bowel syndrome (IBS) may become more prevalent in individuals who have undergone vagus nerve cutting procedures.
It is crucial to consult with a medical professional to weigh the potential benefits against the risks before considering such a procedure. While cutting the vagus nerve may be necessary in specific medical conditions, understanding the potential consequences is vital in making an informed decision about one’s health.
Medical Perspectives on Vagus Nerve Cutting
Medical professionals approach the cutting of the vagus nerve with caution, as it is a significant decision that requires thorough evaluation and consideration of alternatives.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and respiratory function. It is a long and complex nerve that extends from the brainstem to multiple organs throughout the body.
When considering vagus nerve cutting as a medical intervention, healthcare professionals carefully weigh the potential benefits against the risks and complications that may arise. While it can provide relief for certain health conditions, such as epilepsy or treatment-resistant depression, it is not a decision to be taken lightly.
Risks and Complications in Medical Practice
While the cutting of the vagus nerve can provide relief for certain health conditions, it is not without risks and complications. Possible complications may include infection, damage to nearby structures, or adverse reactions to anesthesia. These risks highlight the importance of thorough preoperative evaluation and careful surgical technique to minimize potential harm.
Additionally, healthcare providers must consider the long-term consequences of vagus nerve cutting. The vagus nerve plays a vital role in maintaining homeostasis and regulating various bodily functions. Severing this nerve may lead to unintended consequences, such as impaired digestion, altered heart rate variability, or changes in mood and cognition.
It is crucial to discuss these potential risks with a healthcare professional before making any decisions. Patients should be fully informed about the potential benefits and drawbacks of vagus nerve cutting, allowing them to make an educated decision based on their unique circumstances and medical history.
Ethical Considerations in Vagus Nerve Surgery
Vagus nerve cutting is a serious medical procedure that raises ethical considerations. Due to its potential impact on an individual’s well-being, it is important for medical professionals to ensure that the procedure is performed with the utmost care and only in cases where the benefits truly outweigh the risks.
Healthcare providers should engage in open and transparent discussions with patients, helping them make informed decisions about their treatment options. Informed consent is of paramount importance, as patients need to understand the potential consequences and alternatives available to them.
Furthermore, medical professionals must consider the long-term implications of vagus nerve cutting on a patient’s quality of life. While it may provide relief for certain conditions, it is essential to assess the potential impact on the patient’s overall well-being and ensure that the procedure aligns with their values and goals.
Ethical guidelines and principles, such as beneficence, non-maleficence, and respect for autonomy, should guide healthcare professionals in their decision-making process. The ultimate goal is to prioritize the patient’s best interests while upholding the principles of medical ethics.
Alternatives to Cutting the Vagus Nerve
While cutting the vagus nerve may be a viable option in specific cases, there are alternative treatments available for various conditions affecting the vagus nerve and the stomach.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating many bodily functions, including digestion, heart rate, and breathing. When the vagus nerve is damaged or malfunctioning, it can lead to a range of symptoms and conditions, such as gastroparesis, epilepsy, and depression.
Non-Surgical Treatments for Vagus Nerve Disorders
Depending on the underlying condition, alternative treatments such as medication, dietary modifications, or lifestyle changes may be effective in managing symptoms and improving quality of life. For example, individuals with gastroparesis, a condition characterized by delayed stomach emptying, may benefit from medications that stimulate gastric motility or dietary adjustments that involve consuming smaller, more frequent meals.
Furthermore, certain lifestyle changes can positively impact the vagus nerve’s function. Engaging in regular exercise, practicing stress-reducing techniques like meditation or yoga, and getting sufficient sleep can all contribute to maintaining a healthy vagus nerve.
Future Research and Innovations in Vagus Nerve Treatment
Ongoing research in the field of neurology and gastrointestinal medicine is continually advancing our understanding of the vagus nerve and its functions. Scientists and medical professionals are exploring innovative approaches to treat vagus nerve disorders without resorting to surgical interventions.
One promising area of research involves the use of neuromodulation techniques, such as vagus nerve stimulation (VNS). VNS involves the implantation of a device that delivers electrical impulses to the vagus nerve, helping to regulate its activity. This therapy has shown promising results in treating epilepsy, depression, and even inflammatory bowel disease.
Another avenue of exploration is the development of targeted drug therapies that specifically address the underlying causes of vagus nerve disorders. By targeting the molecular pathways involved in the dysfunction of the vagus nerve, researchers hope to develop more effective and personalized treatments.
Additionally, advancements in non-invasive techniques, such as transcutaneous vagus nerve stimulation (tVNS), are being investigated. tVNS involves applying electrical stimulation to the skin overlying the vagus nerve, offering a potential alternative to surgical procedures.
As our understanding of the vagus nerve continues to deepen, it is likely that new and less invasive treatment options will emerge. These advancements offer hope for individuals with vagus nerve disorders, providing them with alternatives to cutting the nerve and improving their overall well-being.
In Conclusion
The decision to cut the vagus nerve to the stomach should not be taken lightly. It is a complex surgical procedure with potential implications for an individual’s health and well-being. Before considering such a procedure, it is crucial to consult with a medical professional who can provide expert guidance and weigh the potential risks and benefits. The vagus nerve, with its intricate connection to the stomach and the broader body, plays a vital role in maintaining optimal health and should be treated with utmost care.