The vagus nerve, also known as the “wandering nerve,” is a crucial component of the body’s intricate nervous system. It plays a significant role in regulating various bodily functions, including digestion. But what happens if this nerve is cut? In this article, we will delve into the consequences of cutting the vagus nerve and explore the intricate relationship between this nerve and the stomach.
Understanding the Vagus Nerve
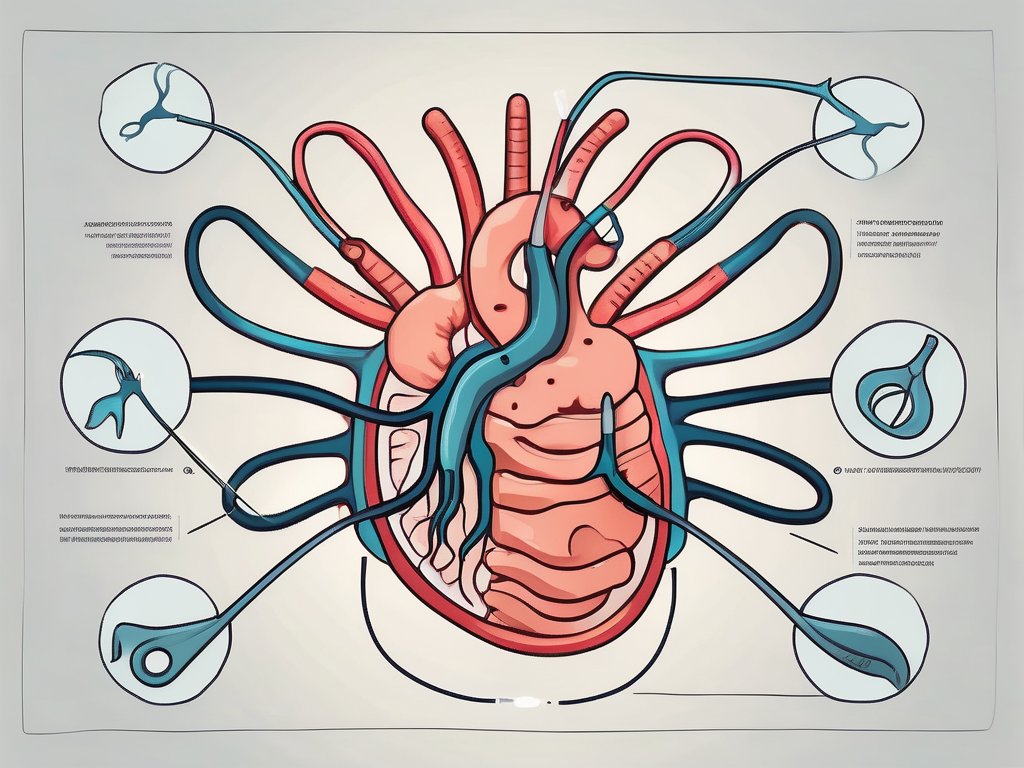
The vagus nerve is the largest and most complex cranial nerve in the body. It originates in the brainstem and extends down to the abdomen, touching and innervating various organs along the way. This nerve is responsible for carrying vital information between the brain and different parts of the body, controlling important functions such as heart rate, breathing, and digestion.
But what exactly does the vagus nerve do? Let’s dive deeper into its role in the body.
The Role of the Vagus Nerve in the Body
The vagus nerve serves as the primary means of communication between the brain and the body’s internal organs. It plays a critical role in regulating the parasympathetic nervous system, which is responsible for rest, relaxation, and digestion. When the vagus nerve is functioning optimally, it ensures the smooth coordination of these bodily functions.
When we think about the vagus nerve, we often associate it with the “rest and digest” response. This refers to the parasympathetic nervous system’s activation, which is controlled by the vagus nerve. When we are in a state of relaxation, the vagus nerve helps slow down our heart rate, lower blood pressure, and promote digestion.
But the vagus nerve’s influence extends beyond just these functions. It also plays a role in regulating inflammation in the body. When the vagus nerve is activated, it releases anti-inflammatory molecules that help reduce the body’s inflammatory response. This is why techniques like deep breathing and meditation, which stimulate the vagus nerve, can have a calming effect on the body.
The Vagus Nerve and the Stomach
The vagus nerve is intricately connected to the stomach, playing a pivotal role in regulating its functions. When food enters the stomach, the vagus nerve stimulates the release of gastric acid and digestive enzymes. It also facilitates the movement of food through the digestive tract, ensuring proper digestion and absorption of nutrients.
But the vagus nerve’s involvement in stomach function goes beyond digestion. It also plays a role in signaling feelings of fullness and satiety to the brain. When the stomach stretches as it fills with food, the vagus nerve sends signals to the brain to indicate that we are satisfied and should stop eating. This communication between the stomach and the brain helps regulate our appetite and prevent overeating.
In addition to its role in digestion and appetite regulation, the vagus nerve also influences the gut-brain axis. This bidirectional communication pathway between the gut and the brain plays a crucial role in our overall well-being. The vagus nerve helps transmit signals from the gut to the brain, influencing our mood, emotions, and even cognitive function.
Understanding the complexities of the vagus nerve and its interactions with various organs in the body is essential for appreciating the intricate balance that exists within us. From regulating heart rate to facilitating digestion and influencing our emotional well-being, the vagus nerve truly is a remarkable part of our physiology.
The Impact of Cutting the Vagus Nerve
The vagus nerve plays a crucial role in the communication between the brain and the stomach. When this nerve is severed or damaged, it disrupts the smooth flow of information, leading to various effects on the stomach’s functionality.
Immediate Effects on the Stomach
One of the immediate effects of cutting the vagus nerve is the compromised ability of the stomach to secrete sufficient gastric acid and digestive enzymes. These substances are essential for breaking down food and facilitating the absorption of nutrients.
As a result of this disruption, individuals may experience a reduced appetite. The signals that typically indicate hunger to the brain may be altered, leading to a decreased desire to eat. This can have implications for overall nutrition and weight management.
In addition to a reduced appetite, impaired digestion is another immediate effect. Without the proper stimulation from the vagus nerve, the stomach may struggle to break down food effectively. This can result in symptoms such as bloating, discomfort, and indigestion.
Furthermore, the process of emptying the stomach may become slower when the vagus nerve is cut. Normally, the nerve helps coordinate the movement of food through the digestive system. Without its influence, the stomach may take longer to empty its contents, leading to feelings of fullness and delayed digestion.
Long-term Consequences for Digestion
The impact of cutting the vagus nerve extends beyond the immediate effects and can have significant long-term consequences for digestion.
Without the proper stimulation and regulation from the vagus nerve, the stomach may struggle to break down food effectively over time. This can result in chronic symptoms such as persistent bloating, indigestion, and discomfort after meals.
In addition to these uncomfortable symptoms, cutting the vagus nerve can also lead to nutrient deficiencies. The impaired digestion and absorption of nutrients can prevent the body from adequately extracting essential vitamins, minerals, and other vital substances from food. This can have a cascading effect on overall health and well-being.
It is crucial for individuals who have had their vagus nerve cut or damaged to consult with a medical professional. They can provide guidance on managing the potential complications and offer strategies to support digestion and overall health.
Medical Procedures Involving the Vagus Nerve
Vagus Nerve Stimulation
Vagus Nerve Stimulation (VNS) is a medical procedure that involves implanting a device that electrically stimulates the vagus nerve. This therapy is primarily used to control seizures in individuals with epilepsy. The vagus nerve, also known as the “wandering nerve,” is a crucial component of the parasympathetic nervous system, responsible for regulating various bodily functions including heart rate, digestion, and mood.
During VNS, a small device is surgically implanted under the skin, typically in the chest area. This device is connected to a wire that is carefully wrapped around the vagus nerve in the neck. Once the device is activated, it delivers mild electrical impulses to the vagus nerve at regular intervals, helping to regulate abnormal electrical activity in the brain that can lead to seizures.
While VNS does not involve cutting the vagus nerve, it can still impact the function of the nerve and, consequently, affect stomach function. The vagus nerve plays a crucial role in the communication between the brain and the digestive system. It helps regulate the release of stomach acid, the movement of food through the digestive tract, and the sensation of fullness after a meal. Therefore, the electrical stimulation provided by VNS can influence these processes, potentially leading to changes in appetite, digestion, and even weight.
Vagotomy: Purpose and Procedure
Vagotomy is a surgical procedure that involves cutting or removing a part of the vagus nerve. It is typically performed to manage specific gastrointestinal conditions, such as ulcers or excessive stomach acid production. The vagus nerve plays a crucial role in stimulating the production of gastric acid in the stomach. However, in certain cases, excessive acid production can lead to the development of ulcers or other digestive disorders.
During a vagotomy, the surgeon carefully identifies and isolates the section of the vagus nerve that needs to be treated. Depending on the specific condition being addressed, different techniques may be used to cut or remove the targeted portion of the nerve. This procedure aims to reduce the production of gastric acid and alleviate related symptoms, such as abdominal pain, heartburn, and indigestion.
However, it is important to note that this procedure carries its own set of risks and implications for digestion. While vagotomy can effectively reduce acid production, it may also disrupt the normal functioning of the digestive system. The vagus nerve plays a crucial role in coordinating the movement of food through the digestive tract, stimulating the release of digestive enzymes, and regulating the sensation of hunger and fullness. Therefore, altering the vagus nerve’s function through vagotomy can potentially lead to changes in digestion, nutrient absorption, and appetite regulation.
It is essential for individuals considering vagotomy to thoroughly discuss the potential risks, benefits, and long-term implications with their healthcare provider. The decision to undergo vagotomy should be carefully weighed against alternative treatment options and the specific needs of the patient.
Potential Risks and Complications
Risks Associated with Vagus Nerve Damage
When the vagus nerve is cut or damaged, certain risks and complications may arise. These can include impaired digestion, difficulty in maintaining a healthy weight, and an increased susceptibility to gastrointestinal infections. As each individual’s circumstances differ, it is crucial to consult with a healthcare professional to understand the specific risks involved.
Impaired digestion is one of the primary risks associated with vagus nerve damage. The vagus nerve plays a crucial role in regulating the digestive system, including the production of stomach acid, the release of digestive enzymes, and the movement of food through the gastrointestinal tract. When the nerve is damaged, these processes can be disrupted, leading to symptoms such as bloating, indigestion, and constipation.
Another potential risk is difficulty in maintaining a healthy weight. The vagus nerve is involved in regulating appetite and satiety signals, which help to control food intake and energy balance. Damage to the nerve can disrupt these signals, leading to increased hunger and a decreased feeling of fullness. This can make it challenging to maintain a healthy weight and may contribute to weight gain or difficulty in losing weight.
In addition to impaired digestion and weight management issues, vagus nerve damage can also result in an increased susceptibility to gastrointestinal infections. The vagus nerve plays a role in immune system regulation, helping to coordinate the body’s response to pathogens. When the nerve is damaged, this coordination can be compromised, making it harder for the immune system to effectively fight off infections in the gastrointestinal tract. This can lead to a higher risk of developing conditions such as gastroenteritis or bacterial overgrowth.
Managing Complications Post-Vagotomy
If you have undergone vagotomy, it is important to work closely with your healthcare team to manage any complications that may arise. They can provide guidance on dietary modifications, supplementation, and other strategies to optimize digestion and minimize potential side effects.
Dietary modifications can play a significant role in managing complications post-vagotomy. Your healthcare team may recommend specific dietary changes, such as consuming smaller, more frequent meals to aid digestion, avoiding foods that are difficult to digest, and incorporating fiber-rich foods to promote regular bowel movements. They may also suggest avoiding certain beverages, such as alcohol and caffeine, as these can irritate the gastrointestinal tract and exacerbate symptoms.
In some cases, supplementation may be necessary to address nutrient deficiencies that can occur as a result of impaired digestion. Your healthcare team may recommend specific supplements, such as digestive enzymes or probiotics, to support digestion and promote a healthy gut environment. They will closely monitor your nutrient levels and adjust supplementation as needed to ensure optimal health.
Alongside dietary modifications and supplementation, other strategies may be employed to manage complications post-vagotomy. These can include lifestyle changes, such as regular exercise to support weight management and improve overall gastrointestinal function. Your healthcare team may also recommend stress management techniques, as stress can worsen symptoms and impact digestion. Additionally, they may prescribe medications to alleviate specific symptoms or address underlying conditions that may contribute to complications.
Recovery and Adaptation
The Body’s Response to Vagus Nerve Damage
Following vagus nerve damage, the body may undergo a period of adaptation. The remaining branches of the vagus nerve and other parts of the autonomic nervous system may compensate to some extent, restoring certain aspects of stomach function. However, it is essential to approach this process with patience and seek appropriate medical guidance as needed.
During the recovery process, the body’s intricate network of nerves and cells work tirelessly to restore normal function to the stomach. The remaining branches of the vagus nerve, like dedicated messengers, send signals to the stomach, attempting to bridge the gap left by the damaged portion. This remarkable ability of the body to adapt and compensate is a testament to its resilience.
As the body adapts, it may take time for the stomach to regain its full functionality. The process can be compared to a symphony, with different parts of the autonomic nervous system playing their unique roles to restore harmony. The sympathetic nervous system, responsible for the body’s fight-or-flight response, may step in to support the compromised vagus nerve, ensuring that essential functions continue to operate.
Living with Altered Stomach Function
If you experience long-term alterations in stomach function due to vagus nerve damage, it is important to seek support and guidance from a healthcare professional. They can help you develop strategies to manage symptoms, adjust your diet, and ensure optimal overall health.
Living with altered stomach function can present unique challenges that require careful consideration. It is crucial to work closely with a healthcare professional who can provide personalized guidance and support. They can help you navigate the intricacies of managing symptoms and adjusting your diet to ensure that you receive the necessary nutrients while minimizing discomfort.
Additionally, a healthcare professional can help you explore alternative therapies and treatments that may aid in the recovery process. From acupuncture to specialized exercises, there are various approaches that can complement traditional medical interventions and promote healing.
Furthermore, seeking support from others who have experienced similar challenges can be invaluable. Support groups and online communities can provide a safe space to share experiences, exchange tips, and find emotional support. Connecting with others who understand the journey can help alleviate feelings of isolation and empower you to take control of your health.
Remember, while living with altered stomach function may present ongoing challenges, it is important to remain hopeful and proactive in your approach. With the right support and guidance, you can adapt to these changes and continue to live a fulfilling and healthy life.
Prevention and Protection
The vagus nerve plays a crucial role in the functioning of the human body, particularly in regulating digestion. It is responsible for transmitting signals between the brain and various organs, including the stomach. Therefore, it is essential to prioritize the protection of the vagus nerve whenever possible to maintain optimal health.
Ways to Protect the Vagus Nerve
There are several ways to protect the vagus nerve and ensure its smooth functioning. One of the most important factors is maintaining a healthy lifestyle. This includes eating a balanced diet that is rich in nutrients and avoiding excessive consumption of processed foods, which can negatively impact nerve health.
In addition to a healthy diet, managing stress is crucial for protecting the vagus nerve. Chronic stress can lead to inflammation and damage to the nerve, affecting its ability to transmit signals effectively. Engaging in stress-reducing activities such as meditation, yoga, or deep breathing exercises can help promote vagus nerve health.
Furthermore, it is important to avoid behaviors or substances that can harm nerve health. This includes limiting alcohol consumption, avoiding smoking, and minimizing exposure to toxins and pollutants. These harmful substances can impair the functioning of the vagus nerve and increase the risk of nerve damage.
Importance of Regular Check-ups and Monitoring
Regular check-ups with a healthcare professional are crucial, especially if you have a pre-existing condition or have undergone vagus nerve-related procedures. These check-ups allow for ongoing monitoring of the nerve’s health and can help identify any potential complications early on.
During these check-ups, healthcare professionals may perform tests and examinations to assess the functioning of the vagus nerve. This can include measuring heart rate variability, assessing gastrointestinal motility, or conducting nerve conduction studies. By closely monitoring the vagus nerve, healthcare professionals can detect any abnormalities or signs of damage, enabling timely intervention and management.
Moreover, regular check-ups provide an opportunity for healthcare professionals to educate patients on the importance of vagus nerve health and offer guidance on lifestyle modifications that can support its well-being. They can also address any concerns or questions patients may have, ensuring they feel informed and empowered in managing their nerve health.
In conclusion, the vagus nerve is a vital component of the human body, particularly in regulating digestive processes. Protecting and prioritizing its health is crucial for overall well-being. By maintaining a healthy lifestyle, managing stress, and avoiding behaviors or substances that can harm nerve health, individuals can contribute to the optimal functioning of the vagus nerve. Additionally, regular check-ups and monitoring with healthcare professionals play a significant role in identifying and managing potential complications effectively. If you are facing vagus nerve-related issues, it is essential to consult with a healthcare professional who can provide guidance and support tailored to your specific needs.