Gastroparesis is a condition that affects the normal movement of food through the stomach. It occurs when the vagus nerve, which plays a crucial role in digestion, is damaged or cut. Understanding the connection between gastroparesis and the vagus nerve is essential in addressing the impact of this condition on the digestive system.
Understanding Gastroparesis and the Vagus Nerve
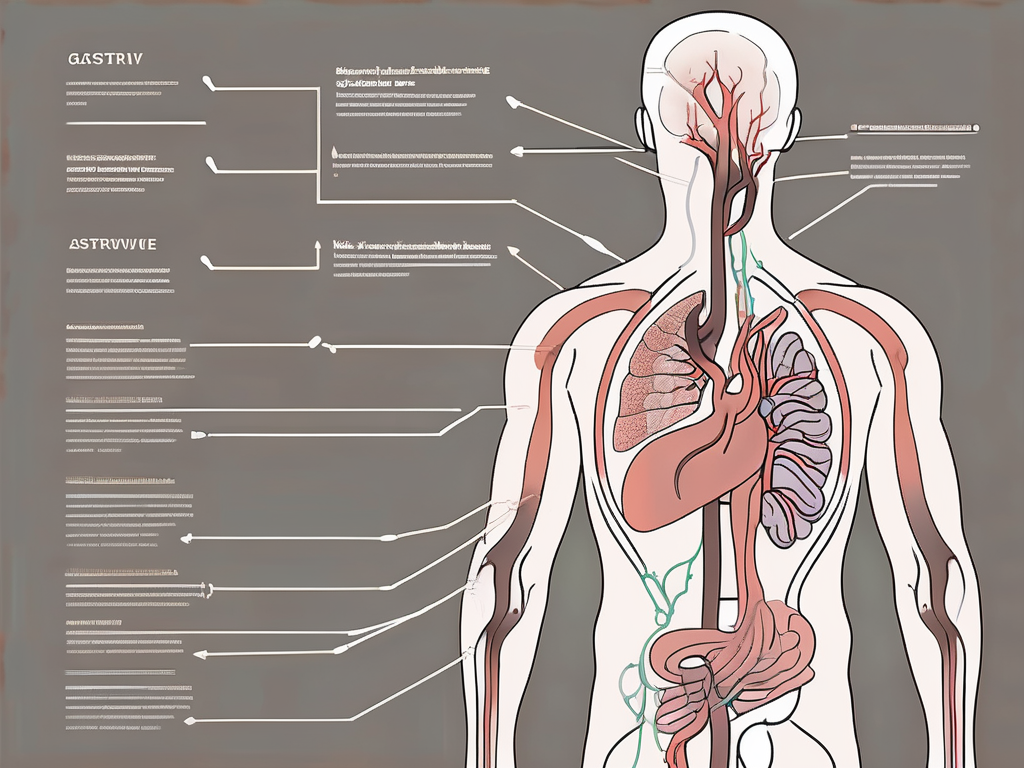
The vagus nerve is the longest cranial nerve in the body, running from the brainstem all the way down to the abdomen. It has a vital role in regulating various bodily functions, including digestion. When the vagus nerve is functioning correctly, it sends signals to the stomach muscles to contract and move food into the small intestine. However, if the vagus nerve is damaged or cut, these signals can be disrupted, leading to gastroparesis.
The Role of the Vagus Nerve in Digestion
During the process of digestion, the vagus nerve communicates with the stomach muscles, controlling their contractions to allow food to be properly broken down and moved along the digestive tract. It also regulates the release of stomach acid and digestive enzymes necessary for optimal digestion.
When food enters the stomach, the vagus nerve senses its presence and sends signals to the muscles in the stomach wall, initiating a series of contractions known as peristalsis. These contractions help to mix the food with stomach acid and digestive enzymes, breaking it down into smaller particles. The vagus nerve ensures that these contractions occur in a coordinated manner, allowing for efficient digestion.
In addition to controlling stomach contractions, the vagus nerve also plays a role in regulating the release of stomach acid and digestive enzymes. It communicates with the cells in the stomach lining, known as parietal cells and chief cells, to stimulate the production and secretion of hydrochloric acid and digestive enzymes, respectively. These substances are essential for breaking down food and extracting nutrients.
Furthermore, the vagus nerve is involved in the regulation of the lower esophageal sphincter (LES), a muscular ring that separates the esophagus from the stomach. It helps to keep the LES closed when food is not being swallowed, preventing stomach acid from flowing back into the esophagus and causing heartburn.
Gastroparesis: A Brief Overview
Gastroparesis is a chronic condition characterized by delayed stomach emptying. Individuals with gastroparesis experience a range of symptoms, including nausea, vomiting, bloating, and abdominal pain. When the vagus nerve is damaged or cut, gastroparesis may develop, causing disruptions in the normal digestive process.
There are various causes of vagus nerve damage, including diabetes, surgery, viral infections, and certain medications. In diabetic individuals, high blood sugar levels can damage the nerves, including the vagus nerve. Surgical procedures that involve the removal or manipulation of the stomach or nearby organs can also inadvertently damage the vagus nerve. Additionally, viral infections, such as herpes or Epstein-Barr virus, can cause inflammation and damage to the nerve.
Gastroparesis can significantly impact a person’s quality of life, as it can lead to malnutrition, dehydration, and weight loss. Treatment options for gastroparesis include dietary changes, medications to stimulate stomach contractions, and in severe cases, surgical interventions such as gastric electrical stimulation or pyloroplasty.
In conclusion, the vagus nerve plays a crucial role in the regulation of digestion. When it is functioning properly, it ensures that food is properly broken down and moved along the digestive tract. However, damage to the vagus nerve can lead to gastroparesis, a condition characterized by delayed stomach emptying. Understanding the role of the vagus nerve in digestion and the development of gastroparesis can help individuals manage their symptoms and seek appropriate treatment.
The Impact of Vagus Nerve Damage on Gastroparesis
When the vagus nerve is damaged or cut, several factors contribute to the development of gastroparesis. Understanding how these factors interact can shed light on the complexities of this condition.
Gastroparesis is a condition characterized by delayed emptying of the stomach, resulting in various symptoms and complications. The vagus nerve plays a crucial role in regulating stomach contraction and emptying. When this nerve is damaged, the signals that should coordinate the movement of food through the digestive tract become ineffective, leading to the development of gastroparesis.
How Vagus Nerve Damage Occurs
Vagus nerve damage can occur due to various reasons, such as surgery, injury, or medical conditions like diabetes. Surgical procedures that involve the removal or manipulation of tissues near the vagus nerve can inadvertently cause damage. Additionally, traumatic injuries, such as those sustained in accidents or falls, can also result in nerve damage.
Diabetes, a chronic condition characterized by high blood sugar levels, is a common cause of vagus nerve damage. Prolonged exposure to high blood sugar levels can lead to nerve damage throughout the body, including the vagus nerve. Over time, this damage can impair the nerve’s ability to transmit signals effectively, leading to gastroparesis.
Symptoms and Complications of Gastroparesis with Vagus Nerve Damage
Individuals with gastroparesis resulting from vagus nerve damage often experience a range of troubling symptoms. Nausea and vomiting are prevalent symptoms, occurring frequently and sometimes without warning. The delayed emptying of the stomach can cause food to remain in the digestive system for longer periods, leading to feelings of fullness even after consuming small meals, a condition known as early satiety.
For individuals with diabetes, gastroparesis can further complicate blood sugar management. The unpredictable variations in stomach emptying can result in erratic absorption of glucose from the digestive tract, leading to fluctuations in blood sugar levels. This can make it challenging for individuals with diabetes to maintain stable blood sugar control, requiring frequent adjustments in medication and dietary management.
If left unmanaged, gastroparesis can lead to malnutrition and dehydration. The delayed emptying of the stomach can hinder the absorption of essential nutrients, depriving the body of vital vitamins, minerals, and calories. This can result in weight loss, weakness, and fatigue. Additionally, the prolonged presence of food in the digestive system can increase the risk of bacterial overgrowth and infections, further exacerbating the complications associated with gastroparesis.
Medical Procedures Involving the Vagus Nerve
In some cases, surgical interventions may be considered to manage vagus nerve damage and alleviate gastroparesis symptoms. These procedures aim to restore or improve vagus nerve functionality.
One such procedure is vagus nerve stimulation (VNS), which involves the implantation of a small device that delivers electrical impulses to the vagus nerve. This stimulation can help regulate the signals sent between the brain and the digestive system, potentially improving gastric motility and reducing symptoms of gastroparesis.
Another surgical option is vagotomy, which involves cutting or removing a portion of the vagus nerve. This procedure is typically reserved for severe cases where other treatment options have been ineffective. By interrupting the signals sent by the vagus nerve, vagotomy can help reduce the symptoms of gastroparesis, such as nausea, vomiting, and bloating.
Risks and Benefits of Vagus Nerve Surgery
Vagus nerve surgery is a complex procedure that carries its own set of risks and benefits. It is important for individuals considering this option to have a thorough understanding of both the potential advantages and potential drawbacks.
One of the main benefits of vagus nerve surgery is the potential for significant symptom improvement. For individuals with severe gastroparesis symptoms that have not responded to other treatments, surgery may offer a chance to regain a better quality of life. By restoring or improving vagus nerve functionality, surgical interventions can help regulate gastric motility and reduce symptoms such as early satiety, abdominal pain, and malnutrition.
However, like any surgical procedure, vagus nerve surgery also carries certain risks. These can include infection, bleeding, damage to surrounding structures, and the potential for the surgery to not provide the desired level of symptom relief. It is crucial for individuals to have a detailed discussion with their healthcare professional to fully understand the potential risks and benefits of such procedures.
Post-Surgery Care and Management
After undergoing vagus nerve surgery for gastroparesis, patients require diligent post-operative care to support a smooth recovery and maximize the benefits of the procedure.
One important aspect of post-surgery care is dietary modifications. Following surgery, individuals may need to make adjustments to their eating habits to ensure optimal healing and minimize digestive symptoms. This may involve consuming smaller, more frequent meals, avoiding certain foods that can exacerbate gastroparesis symptoms, and working closely with a registered dietitian to develop a personalized meal plan.
Wound care is another crucial aspect of post-surgery management. Patients will need to keep the surgical incision site clean and dry to prevent infection. They may also be advised to avoid activities that could put strain on the incision area, such as heavy lifting or strenuous exercise, until it has fully healed.
Close monitoring of symptoms is essential during the post-operative period. Patients should keep track of any changes or new symptoms they experience and report them to their healthcare team. Regular follow-up appointments will be scheduled to assess the progress of the surgery and make any necessary adjustments to the treatment plan.
In conclusion, vagus nerve surgery is a potential option for individuals with severe gastroparesis symptoms that have not responded to other treatments. While it carries its own set of risks and benefits, it can offer significant symptom relief and improve quality of life. However, it is important for individuals to consult with their healthcare professional to fully understand the potential risks, benefits, and post-surgery care involved in such procedures.
Treatment Options for Gastroparesis with Vagus Nerve Damage
While surgical interventions exist, there are various non-surgical treatment options available to manage gastroparesis symptoms associated with vagus nerve damage. Gastroparesis is a condition characterized by delayed stomach emptying, which can lead to symptoms such as nausea, vomiting, and abdominal pain. The vagus nerve, which controls the movement of food through the digestive tract, can be damaged due to various factors, including diabetes, surgery, or certain medications.
When it comes to treating gastroparesis with vagus nerve damage, a multimodal approach is often recommended. This means that a combination of different treatment strategies is used to address the symptoms and improve the overall quality of life for individuals with this condition.
Medication and Therapies for Gastroparesis
Medication can be prescribed to stimulate stomach contractions and improve digestion in individuals with gastroparesis. Prokinetic agents, such as metoclopramide or domperidone, are commonly used to enhance gastric motility. These medications work by increasing the coordination and strength of stomach contractions, thereby facilitating the movement of food through the digestive system.
In addition to medication, various therapies may also be recommended to help manage symptoms. Electrical stimulation, for example, involves the use of a device that delivers mild electrical impulses to the stomach muscles, promoting contractions and aiding in digestion. Acupuncture, on the other hand, is an alternative therapy that involves the insertion of thin needles into specific points on the body to stimulate the flow of energy and alleviate symptoms.
It is essential to consult with a healthcare professional to determine the most appropriate treatment plan for gastroparesis with vagus nerve damage. They will consider factors such as the severity of symptoms, underlying causes, and individual patient preferences before recommending a specific course of action.
Lifestyle Changes to Manage Gastroparesis Symptoms
Implementing certain lifestyle modifications can greatly impact the management of gastroparesis symptoms. These changes aim to alleviate symptoms, improve digestion, and enhance overall well-being. Here are some lifestyle recommendations that may be beneficial:
- Consuming smaller, more frequent meals: Instead of having three large meals, individuals with gastroparesis are often advised to eat smaller, more frequent meals throughout the day. This approach helps to reduce the amount of food in the stomach at any given time, making it easier to digest.
- Avoiding foods that are difficult to digest: Certain foods can exacerbate gastroparesis symptoms and should be avoided. These may include high-fat foods, fibrous vegetables, and foods that are high in fiber. Working with a registered dietitian can provide valuable guidance in crafting a suitable meal plan that meets nutritional needs while minimizing symptom flare-ups.
- Maintaining good hydration: Staying hydrated is crucial for individuals with gastroparesis. Adequate fluid intake helps to prevent dehydration and can aid in the movement of food through the digestive system. Sipping on water throughout the day and opting for hydrating beverages such as herbal teas or clear broths can be beneficial.
By making these lifestyle changes, individuals with gastroparesis can have more control over their symptoms and improve their overall quality of life. It is important to note that these modifications should be tailored to each individual’s specific needs and preferences, and guidance from a healthcare professional is highly recommended.
The Future of Gastroparesis Treatment
The field of gastroparesis treatment is continually evolving, with ongoing research and innovations in the realm of vagus nerve therapy. Gastroparesis, a condition characterized by delayed stomach emptying, can cause a range of symptoms such as nausea, vomiting, and abdominal pain. While current treatment options exist, researchers are exploring new ways to stimulate or modulate the vagus nerve to alleviate gastroparesis symptoms.
Innovations in Vagus Nerve Therapy
Researchers are actively investigating various approaches to vagus nerve therapy for gastroparesis. One innovative method being explored is the use of minimally invasive procedures to target specific areas of nerve dysfunction. By precisely stimulating or modulating these areas, researchers hope to restore normal gastric motility and improve symptoms.
In addition to minimally invasive procedures, novel devices are also being developed to deliver targeted therapy to the vagus nerve. These devices may utilize advanced technologies such as neurostimulation or neuromodulation to regulate nerve activity and promote proper stomach emptying. While these advancements hold promise, it is important to remember that they are still in the experimental stages, and further research is required to determine their safety and efficacy.
The Role of Research in Advancing Gastroparesis Treatment
Ongoing scientific research plays a vital role in expanding our understanding of gastroparesis and its relationship with vagus nerve damage. By studying the underlying mechanisms of this condition, researchers can identify potential therapeutic targets and develop innovative treatment strategies.
Collaboration between medical professionals, researchers, and patients is crucial in driving innovation and developing more effective treatment options. Patient participation in clinical trials and research studies provides valuable insights into the lived experience of gastroparesis and helps shape future treatment approaches.
Furthermore, advancements in technology and imaging techniques allow researchers to better visualize and analyze the vagus nerve and its interactions with the digestive system. This enhanced understanding of the nerve’s function and connectivity paves the way for more targeted and personalized therapies.
In conclusion, gastroparesis associated with vagus nerve damage disrupts the normal digestive process, leading to delayed stomach emptying and various symptoms. While surgical interventions and medications can offer options for management, ongoing research and innovations in vagus nerve therapy hold promise for the future of gastroparesis treatment.
Consulting with a doctor is essential to assess individual circumstances and explore the available options to effectively manage this condition. The continuous advancements in vagus nerve therapy offer hope for future innovations in gastroparesis treatment, ultimately improving the quality of life for individuals living with this challenging condition.