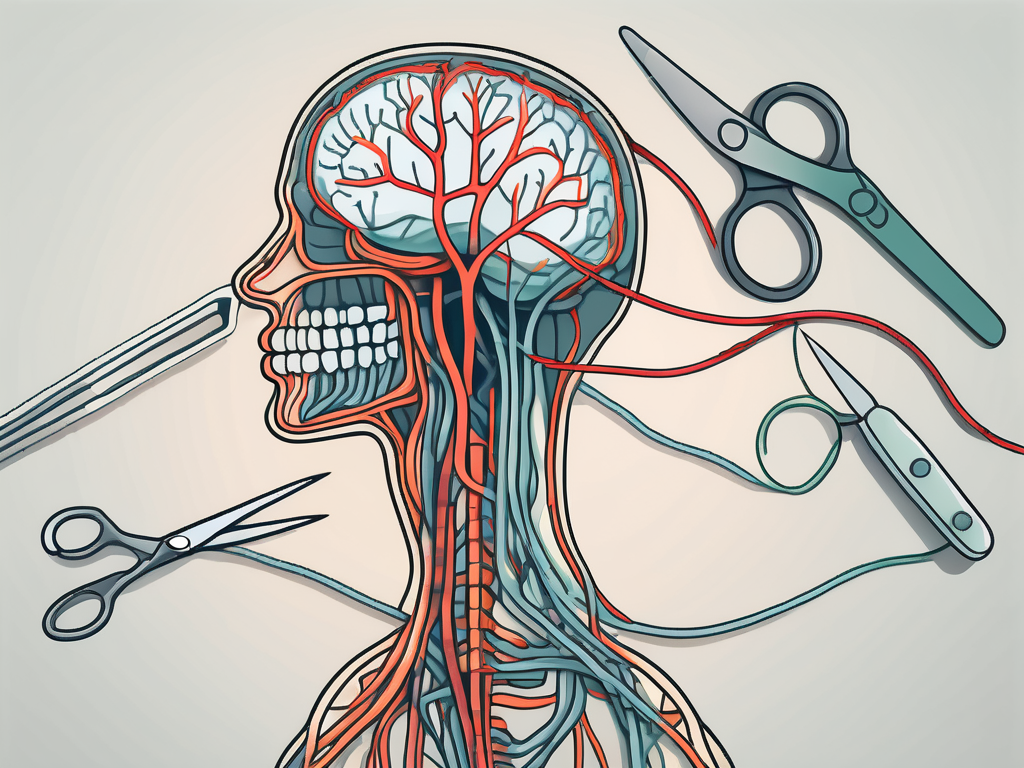
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions. It extends from the brainstem down to the abdomen, connecting with the major organs along the way. But have you ever wondered what would happen if the vagus nerve was cut? In this article, we will explore the fascinating world of the vagus nerve and delve into the possible consequences of severing this vital connection within our bodies.
Understanding the Role of the Vagus Nerve
The vagus nerve is a key component of the autonomic nervous system, which controls vital functions such as heart rate, digestion, respiration, and more. This nerve acts as a communication highway between the brain and various organs, relaying crucial signals that maintain our overall well-being.
The Vagus Nerve and the Autonomic Nervous System
One of the main functions of the vagus nerve is to regulate the parasympathetic response, the branch of the autonomic nervous system responsible for the body’s rest and digest mode. By activating this response, the vagus nerve helps reduce heart rate, increase digestive activities, and stimulate relaxation.
When the body is in a state of rest, the vagus nerve promotes the release of digestive enzymes and increases blood flow to the gastrointestinal tract. This allows for efficient absorption of nutrients and optimal digestion. Additionally, the vagus nerve stimulates the production of saliva, which aids in the breakdown of food and initiates the digestive process.
Furthermore, the vagus nerve plays a crucial role in regulating heart rate. It sends signals to the sinoatrial node, the natural pacemaker of the heart, to slow down the heart rate during periods of rest and relaxation. This helps conserve energy and maintain a steady rhythm, promoting overall cardiovascular health.
Functions of the Vagus Nerve in the Body
Aside from its involvement in the autonomic nervous system, the vagus nerve also plays a role in other essential bodily functions. It aids in the release of important neurotransmitters like acetylcholine, which is crucial for muscle movement, memory, and attention.
Acetylcholine, released by the vagus nerve, acts as a messenger between nerve cells and muscles, allowing for smooth and coordinated movements. This neurotransmitter is particularly important in the functioning of the diaphragm, the main muscle responsible for respiration. The vagus nerve ensures that the diaphragm contracts and relaxes rhythmically, facilitating the process of breathing.
In addition to its role in motor function, the vagus nerve is also involved in the regulation of inflammation and immune response. It communicates with immune cells, releasing anti-inflammatory signals that help modulate the body’s immune system. This intricate connection between the vagus nerve and the immune system highlights the importance of maintaining a healthy vagal tone for overall well-being.
Furthermore, the vagus nerve has been found to influence our emotional well-being. It acts as a bidirectional pathway, allowing communication between the brain and the gut. This connection, often referred to as the gut-brain axis, plays a significant role in regulating mood, stress response, and even cognitive function. The vagus nerve helps transmit signals related to emotions and stress from the brain to the gut, and vice versa, influencing our overall emotional state.
In conclusion, the vagus nerve is a multifaceted component of the autonomic nervous system. Its functions extend beyond regulating heart rate and digestion. From facilitating smooth muscle movements to modulating inflammation and influencing emotional well-being, the vagus nerve plays a vital role in maintaining our overall health and well-being.
The Anatomy of the Vagus Nerve
To understand the consequences of severing the vagus nerve, it is crucial to comprehend its intricate anatomy.
The vagus nerve, also known as cranial nerve X, is one of the longest and most important nerves in the body. It is a complex network of nerve fibers that plays a vital role in regulating various bodily functions. Let’s explore the anatomy of this fascinating nerve in more detail.
Pathway of the Vagus Nerve
The vagus nerve begins its journey in the brainstem, specifically the medulla oblongata. From there, it travels down through the neck, chest, and abdomen, branching out along the way to connect with organs such as the heart, lungs, and digestive system. This extensive pathway allows the vagus nerve to exert its influence over a wide range of bodily functions.
As the vagus nerve descends through the neck, it gives off several branches that innervate important structures. One such branch, known as the superior laryngeal nerve, supplies sensation to the larynx, enabling us to speak and swallow. Another branch, called the recurrent laryngeal nerve, loops around the aorta and innervates the muscles responsible for vocal cord movement.
Continuing its journey, the vagus nerve enters the thoracic cavity, where it forms connections with the heart and lungs. These connections allow the vagus nerve to regulate heart rate, blood pressure, and respiratory functions. It acts as a crucial link between the brain and these vital organs, ensuring their proper functioning.
As the vagus nerve reaches the abdomen, it further divides into multiple branches that innervate various organs of the digestive system. These branches, known as the anterior and posterior vagal trunks, provide sensory and motor innervation to the stomach, liver, gallbladder, pancreas, and intestines. They play a crucial role in regulating digestion, nutrient absorption, and gut motility.
Branches and Connections of the Vagus Nerve
Throughout its course, the vagus nerve branches out into smaller nerve fibers, forming connections with organs such as the heart, lungs, liver, and intestines. These connections enable the vagus nerve to transmit signals and regulate the activities of these important organs.
One of the most significant branches of the vagus nerve is the cardiac branch. This branch innervates the heart, playing a crucial role in maintaining a steady heart rate and controlling the force of cardiac contractions. It helps to keep our heartbeat regular and ensures adequate blood supply to the body.
Another important branch of the vagus nerve is the pulmonary branch, which provides sensory and motor innervation to the lungs. It helps regulate breathing patterns, ensuring proper oxygenation of the blood and removal of carbon dioxide. Without the vagus nerve’s influence, our respiratory system would not function optimally.
In addition to its cardiac and pulmonary branches, the vagus nerve also forms connections with the liver and intestines. These connections allow it to regulate various aspects of digestion, including the release of digestive enzymes, bile production, and gut motility. The vagus nerve acts as a communication channel between the brain and the digestive system, ensuring efficient digestion and absorption of nutrients.
Overall, the vagus nerve’s intricate anatomy and extensive network of connections make it a vital component of the autonomic nervous system. Its influence over the heart, lungs, and digestive system highlights its importance in maintaining homeostasis and overall well-being.
The Consequences of Cutting the Vagus Nerve
Now, let’s explore what might occur if the vagus nerve were cut or severed.
The vagus nerve, also known as the “wandering nerve,” is a crucial component of the autonomic nervous system. It is responsible for regulating various bodily functions, including heart rate, digestion, breathing, and immune response. Therefore, cutting or severing this nerve can have significant immediate physical effects and long-term health implications.
Immediate Physical Effects
If the vagus nerve were cut, it could have significant immediate physical effects. These may include a rapid increase in heart rate, potential disruptions in digestion, and difficulties in breathing. The vagus nerve plays a vital role in controlling heart rate, so severing it can lead to an unregulated and irregular heartbeat. This can be dangerous and may require immediate medical attention.
In terms of digestion, the vagus nerve helps coordinate the movement of food through the digestive tract and stimulates the release of digestive enzymes. Cutting this nerve can disrupt these processes, leading to issues such as slowed digestion, constipation, or even malabsorption of nutrients.
Furthermore, the vagus nerve is involved in regulating the muscles responsible for breathing. Severing it can result in difficulties in breathing, potentially leading to respiratory problems and a decreased ability to maintain a normal oxygen level in the body.
Additionally, the body’s ability to regulate inflammation and immune response may be compromised. The vagus nerve plays a crucial role in the “inflammatory reflex,” which helps control the body’s immune response and inflammation levels. Cutting this nerve can disrupt this reflex, potentially leading to an overactive immune system and chronic inflammation.
Long-Term Health Implications
The long-term health implications of cutting the vagus nerve can vary depending on the extent and location of the severance. Potential consequences may include gastrointestinal issues, heart rhythm abnormalities, problems with immune regulation, and emotional disturbances.
One of the most common long-term health implications is gastrointestinal issues. As mentioned earlier, the vagus nerve is involved in coordinating digestion. Cutting it can lead to conditions such as gastroparesis, where the stomach muscles do not function properly, resulting in delayed emptying of the stomach. This can cause symptoms like nausea, vomiting, and bloating.
Heart rhythm abnormalities, known as arrhythmias, can also occur as a result of cutting the vagus nerve. The nerve helps regulate the electrical signals that control the heart’s rhythm. Without its influence, the heart may experience irregularities in its beating pattern, potentially leading to palpitations, dizziness, or even more severe cardiac complications.
Problems with immune regulation can arise when the vagus nerve is severed. As mentioned earlier, this nerve plays a role in controlling the body’s immune response. Cutting it can disrupt this regulation, leading to an overactive immune system that may contribute to autoimmune disorders or an increased susceptibility to infections.
Finally, emotional disturbances can occur as a consequence of cutting the vagus nerve. This nerve is involved in the communication between the brain and the body, including the regulation of emotions. Severing it can disrupt this communication, potentially leading to mood swings, anxiety, or even depression.
It is important to note that the effects can differ among individuals, and the severity of these implications may range widely. Each person’s physiology and overall health play a significant role in determining the specific consequences of cutting the vagus nerve.
Medical Procedures Involving the Vagus Nerve
While cutting the vagus nerve is not a standard medical procedure, there are instances where healthcare professionals may intentionally interact with this vital nerve.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It originates in the brainstem and travels down through the neck, chest, and abdomen, innervating various organs along the way. Its branches reach the heart, lungs, stomach, liver, and intestines, playing a crucial role in regulating many bodily functions.
Vagus Nerve Stimulation Therapy
Vagus nerve stimulation (VNS) therapy is a procedure where electrical impulses are delivered to the vagus nerve to help treat certain medical conditions, such as epilepsy or treatment-resistant depression. This therapy aims to modulate nerve activity and restore the balance within the body.
During VNS therapy, a small device called a vagus nerve stimulator is implanted under the skin in the chest area. This device is connected to the vagus nerve through a thin wire, and it delivers regular electrical impulses to the nerve. These impulses can help reduce the frequency and severity of seizures in individuals with epilepsy or alleviate symptoms of depression in those with treatment-resistant depression.
Research has also shown promising results in using VNS therapy for other conditions, including migraines, chronic pain, and even certain psychiatric disorders. The precise mechanisms by which VNS therapy exerts its therapeutic effects are still being studied, but it is believed to involve the modulation of neurotransmitters and the regulation of brain activity.
Risks and Complications of Vagus Nerve Surgery
When the vagus nerve is surgically manipulated, there can be risks and complications involved. These may include infection, damage to surrounding structures, or unintended disruption of nerve signaling. As with any surgical procedure involving critical nerves, it is crucial to consult with a healthcare professional to weigh the potential benefits against the associated risks.
During vagus nerve surgery, the surgeon carefully identifies and isolates the vagus nerve to perform the intended procedure. This may involve making incisions in the neck or chest, depending on the specific condition being treated. While every precaution is taken to minimize the risks, there is always a possibility of complications, such as bleeding, nerve damage, or infection.
It is important for patients considering vagus nerve surgery to have a thorough discussion with their healthcare provider about the potential risks and benefits. Factors such as the severity of the underlying condition, the individual’s overall health, and the availability of alternative treatment options should all be taken into account when making an informed decision.
Recovery and Rehabilitation After Vagus Nerve Damage
For individuals who experience vagus nerve damage, recovery and rehabilitation efforts are essential to regain optimal well-being.
When it comes to recovering from vagus nerve damage, there are various therapeutic approaches that can be employed. These approaches are tailored to the specific functions that have been affected by the damage. Physiotherapy, for example, can be used to target and strengthen muscles that have been weakened due to the nerve damage. Occupational therapy, on the other hand, focuses on helping individuals regain their ability to perform daily activities and tasks. Speech therapy may also be necessary for those who have experienced difficulties with their speech as a result of the nerve damage.
Engaging in these therapeutic approaches is crucial as they can promote nerve regeneration and help restore lost functions to the best extent possible. Through targeted exercises and interventions, individuals can gradually regain control over their bodies and improve their overall well-being.
Therapeutic Approaches for Vagus Nerve Damage
Recovery options for vagus nerve damage may involve targeted physiotherapy, occupational therapy, or speech therapy, depending on the affected functions. Engaging in these therapeutic approaches can help promote nerve regeneration, strengthen related muscles, and restore lost functions to the best extent possible.
Physiotherapy, for instance, often involves a combination of exercises and manual techniques to improve muscle strength and flexibility. This can be particularly beneficial for individuals who have experienced muscle weakness or paralysis due to the nerve damage. Occupational therapy focuses on helping individuals regain their ability to perform activities of daily living, such as dressing, eating, and bathing. By employing adaptive techniques and assistive devices, occupational therapists can empower individuals to regain their independence and improve their quality of life.
Speech therapy, on the other hand, can be instrumental in helping individuals overcome speech difficulties caused by vagus nerve damage. Speech therapists use various techniques and exercises to improve speech clarity, articulation, and overall communication skills. They may also provide strategies to manage any swallowing difficulties that may have arisen as a result of the nerve damage.
Lifestyle Changes and Coping Mechanisms
Coping with the consequences of vagus nerve damage often necessitates lifestyle changes and the adoption of coping mechanisms. It is important to work closely with healthcare professionals, who can provide guidance on managing potential difficulties in digestion, heart rate regulation, inflammation, or emotional well-being.
One of the key lifestyle changes that may be recommended is dietary modifications. Since the vagus nerve plays a vital role in digestion, individuals with vagus nerve damage may need to make adjustments to their diet to ensure optimal digestion and nutrient absorption. This may involve avoiding certain foods that are difficult to digest or incorporating more fiber-rich foods to promote healthy bowel movements.
In addition to dietary changes, stress-reduction techniques can also be beneficial for individuals with vagus nerve damage. Chronic stress can have a negative impact on the body’s ability to heal and recover. Therefore, incorporating relaxation techniques such as deep breathing exercises, meditation, or yoga can help reduce stress levels and promote overall well-being.
Emotional support is another crucial aspect of coping with vagus nerve damage. It is not uncommon for individuals to experience emotional challenges such as anxiety or depression as a result of the nerve damage. Seeking support from loved ones, joining support groups, or engaging in therapy can provide individuals with the necessary tools to navigate these emotional difficulties and improve their mental health.
Overall, recovery and rehabilitation after vagus nerve damage require a comprehensive approach that addresses both the physical and emotional aspects of well-being. By utilizing therapeutic approaches, making lifestyle changes, and seeking support, individuals can enhance their quality of life and regain a sense of control over their bodies.
The Future of Vagus Nerve Research
As we continue to delve into the complexities of the vagus nerve, researchers are uncovering promising avenues for further exploration. Advancements in technology and our understanding of this vital nerve offer hope for the development of emerging treatments and therapies.
Emerging Treatments and Technologies
Emerging treatments and technologies, such as non-invasive vagus nerve stimulation, hold promise for individuals affected by vagus nerve damage or related conditions. These innovative approaches aim to harness the power of the vagus nerve to restore normal bodily functions and improve overall health.
Unanswered Questions in Vagus Nerve Study
Despite our growing knowledge, there are still unanswered questions in the field of vagus nerve study. Scientists are exploring the intricacies of how the vagus nerve contributes to various physiological and psychological processes. By unraveling the mysteries of this remarkable nerve, we can gain further insight into its potential implications for human health and develop more targeted and effective treatments.
In conclusion, the consequences of cutting the vagus nerve can have significant impacts on various bodily functions and overall well-being. While medical procedures involving the vagus nerve exist, they come with their own risks and complications. If you have concerns about your vagus nerve or potential damage, it is vital to consult with a healthcare professional who can provide personalized guidance and explore the available treatment options. With ongoing research and advancements, we are hopeful that a brighter future awaits those affected by vagus nerve-related conditions.