The intricate web of nerves that runs throughout our bodies, like a complex highway system, is truly fascinating. Among these nerves, the vagus nerve holds a special place. But what leads medical professionals to resort to cutting this vital nerve? In this article, we will explore the reasons why the vagus nerve may be cut, the impact it has on the human body, and alternative treatments that are being explored.
Understanding the Vagus Nerve
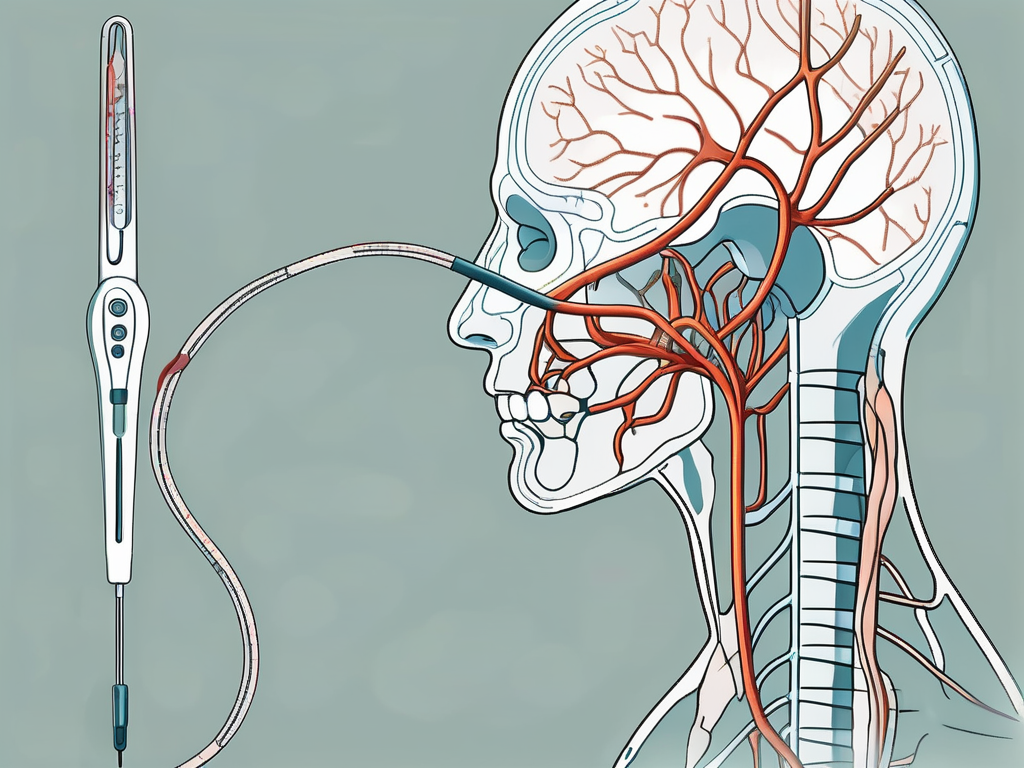
The vagus nerve, also known as the 10th cranial nerve, is the longest and most complex nerve in the human body. It originates in the brainstem and extends throughout the body, reaching various organs, including the heart, lungs, stomach, and intestines. The word “vagus” even translates to “wandering” in Latin, which perfectly describes its extensive reach.
But what exactly does the vagus nerve do? Let’s dive deeper into the anatomy and functions of this fascinating nerve.
Anatomy of the Vagus Nerve
The vagus nerve consists of two main branches: the sensory and motor branches. The sensory branch carries information from the body’s organs to the brain, allowing for communication and regulation. This branch acts as a messenger, transmitting signals about the body’s internal state to the brain, providing crucial feedback for maintaining homeostasis.
On the other hand, the motor branch is responsible for transmitting nerve impulses from the brain to the organs, controlling various functions. It acts as a conductor, orchestrating the intricate symphony of bodily processes. Without the motor branch of the vagus nerve, our organs would be left without guidance, leading to dysfunction and chaos.
Functions of the Vagus Nerve
As a key player in the parasympathetic nervous system, the vagus nerve is involved in numerous vital processes within the body. It regulates heart rate, ensuring that our heartbeat remains steady and coordinated. This function is especially important during moments of stress or physical exertion, when our heart needs to adapt to changing demands.
But the vagus nerve’s influence doesn’t stop at the heart. It also controls lung function, allowing us to breathe effortlessly and efficiently. By sending signals to the muscles responsible for respiration, the vagus nerve ensures that oxygen is delivered to every cell in our body, keeping us energized and alive.
When it comes to digestion, the vagus nerve takes center stage. It plays a crucial role in the intricate dance of the digestive system, coordinating the movement of food through the esophagus, stomach, and intestines. Without the vagus nerve’s guidance, our digestion would be disrupted, leading to discomfort and malabsorption.
But the vagus nerve’s influence extends beyond the physical realm. It also has a profound impact on our emotional well-being. Through its connection with the brain, the vagus nerve influences our mood, stress response, and overall mental health. It acts as a bridge between our body and mind, reminding us that our physical and emotional well-being are deeply intertwined.
Given the vagus nerve’s intricate connection with these vital bodily functions, it’s no wonder that it has become an area of interest for medical professionals. Researchers are constantly uncovering new insights into the vagus nerve’s role in health and disease, paving the way for potential treatments and interventions.
In conclusion, the vagus nerve is a remarkable structure that deserves our attention and appreciation. Its extensive reach and multifaceted functions make it a true marvel of the human body. So the next time you take a deep breath, feel your heart beating, or enjoy a satisfying meal, remember to thank your vagus nerve for its silent but essential contributions.
The Science Behind Vagus Nerve Cutting
When other treatments fail, cutting the vagus nerve may be considered as a last resort. This procedure, known as vagotomy, involves surgically severing or removing a portion of the vagus nerve. While this may seem extreme, the science behind it offers an understanding of its potential efficacy.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the parasympathetic nervous system. It plays a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. By cutting or severing the vagus nerve, the normal transmission of signals between the brain and the affected organs is disrupted, leading to a reduction in symptoms associated with certain medical conditions.
The Medical Procedure Explained
Vagotomy can be performed in different ways, depending on the specific circumstances. The most common type, known as selective vagotomy, targets specific branches of the vagus nerve to minimize potential side effects. This approach aims to achieve the desired therapeutic effect while preserving the overall function of the nerve.
In more severe cases, a complete vagotomy may be conducted, involving the removal or complete severing of the nerve. This procedure is typically reserved for situations where other treatment options have proven ineffective or when the condition being treated requires a more extensive intervention.
During the surgical procedure, the patient is placed under general anesthesia to ensure their comfort and safety. The surgeon carefully identifies and isolates the vagus nerve, taking great care to avoid damaging any surrounding structures. Once the nerve is exposed, the surgeon proceeds with either selective or complete vagotomy, depending on the predetermined treatment plan.
Potential Risks and Complications
As with any surgical procedure, there are risks and possible complications associated with vagotomy. It is crucial for individuals considering this treatment option to be well-informed and consult with a medical professional to weigh the potential benefits against the risks and thoroughly understand the implications.
One potential risk of vagotomy is infection, which can occur at the surgical site. To minimize this risk, strict sterile techniques are followed during the procedure, and patients are typically prescribed antibiotics to prevent any post-operative infections.
Bleeding is another possible complication of vagotomy. The surgeon takes precautions to minimize bleeding during the procedure, and any excessive bleeding is promptly addressed. However, in rare cases, additional interventions may be required to control bleeding effectively.
Damage to surrounding nerves is a potential risk during vagotomy. The surgeon must exercise great precision and care to avoid inadvertently damaging nearby structures. Pre-operative imaging studies and a thorough understanding of the anatomy help guide the surgeon in performing the procedure safely.
Changes in bowel habits may occur following vagotomy. The vagus nerve plays a significant role in regulating digestive functions, and disrupting its normal function can lead to alterations in bowel movements. Patients should be aware of this potential side effect and discuss it with their healthcare provider.
It is important to note that while vagotomy may offer relief for certain conditions, it is not without potential risks and complications. Each individual’s case is unique, and a thorough evaluation by a medical professional is necessary to determine the appropriateness of this procedure.
Reasons for Cutting the Vagus Nerve
While vagotomy is not a common procedure, there are specific medical situations where it may be considered as a treatment option. Let us delve into two common conditions where cutting the vagus nerve can make a significant difference:
Treating Epilepsy
Epilepsy, a neurological disorder characterized by recurrent seizures, can severely impact an individual’s quality of life. In cases where anti-seizure medications and other treatments prove ineffective, cutting the vagus nerve may be considered as a potential solution. By disrupting the abnormal electrical activity in the brain, vagotomy has been shown to reduce the frequency and severity of seizures in some individuals.
When it comes to treating epilepsy, vagotomy is typically performed as a last resort. It is reserved for individuals who have not responded to other treatment options and continue to experience frequent seizures. The procedure involves cutting or removing a portion of the vagus nerve, which is responsible for transmitting signals between the brain and various organs in the body.
During the surgery, the vagus nerve is carefully identified and isolated. The surgeon then determines the appropriate section to be cut or removed, taking into consideration the individual’s specific condition. This targeted approach ensures that the procedure is tailored to the patient’s needs, maximizing the chances of success.
Following the surgery, patients may experience some temporary side effects, such as hoarseness, difficulty swallowing, or changes in voice quality. These symptoms usually subside as the body adjusts to the altered nerve function. It is important for patients to closely follow their post-operative care instructions and attend regular follow-up appointments to monitor their progress.
Managing Treatment-Resistant Depression
Treatment-resistant depression can be debilitating and affect every aspect of life. For individuals who do not respond to traditional treatments such as medication and therapy, vagotomy could offer a glimmer of hope. By interrupting the flow of neural signals associated with depression, this procedure has shown promise in alleviating symptoms in certain cases. However, it must be noted that more research is needed before widespread adoption of this approach.
When it comes to managing treatment-resistant depression, vagotomy is still considered an experimental procedure. It is typically reserved for individuals who have exhausted all other treatment options and continue to experience severe depressive symptoms. The procedure aims to disrupt the communication between the brain and the organs influenced by the vagus nerve, potentially providing relief from depression.
During the vagotomy procedure for depression, the surgeon carefully identifies and isolates the vagus nerve. Different techniques can be used to interrupt the nerve’s function, such as electrical stimulation or surgical removal of a portion of the nerve. The specific approach depends on the individual’s condition and the surgeon’s expertise.
After the surgery, patients may experience some temporary side effects, including changes in appetite, sleep patterns, or mood. These effects are typically mild and resolve as the body adjusts to the altered nerve function. It is crucial for patients to have a comprehensive post-operative care plan, which may include therapy, medication adjustments, and regular follow-up appointments to monitor their progress.
The Impact on the Body Post-Procedure
Undergoing vagotomy undoubtedly has a profound impact on the body. While the specific effects vary from person to person, there are some common changes and adjustments that one can expect both physically and mentally.
When it comes to physical changes and adjustments after vagotomy, the body undergoes a period of adaptation that can be quite significant. Digestion, for instance, may be altered, with some individuals experiencing changes in bowel movements or the need for dietary modifications. This means that individuals may have to make adjustments to their eating habits and carefully monitor their dietary intake to ensure optimal digestion and nutrition.
In addition to changes in digestion, vagotomy can also have an impact on heart rate regulation and lung function. This means that ongoing monitoring and adjustments may be necessary to ensure that these vital bodily functions are properly regulated. Medical professionals will work closely with individuals who have undergone vagotomy to manage these changes and minimize potential disruptions to their overall health and well-being.
While the physical changes and adjustments are significant, it is also important to consider the psychological implications of undergoing vagotomy. Living with a chronic condition and undergoing any surgical procedure can take a toll on one’s mental well-being. It is essential for individuals who have undergone vagotomy to receive the necessary emotional support and therapy to help them navigate the challenges that may arise.
Mental health professionals can play a crucial role in ensuring a holistic approach to care for individuals who have undergone vagotomy. They can provide the necessary support and guidance to help individuals cope with the emotional and psychological impact of the procedure. This may involve techniques such as cognitive-behavioral therapy, which can help individuals develop coping strategies and manage any anxiety or depression that may arise.
Furthermore, support groups can also be beneficial for individuals who have undergone vagotomy. These groups provide a safe space for individuals to share their experiences, exchange advice, and find solace in knowing that they are not alone in their journey. Connecting with others who have undergone similar procedures can provide a sense of community and understanding that can be invaluable in the recovery process.
In conclusion, undergoing vagotomy has a significant impact on both the physical and psychological aspects of an individual’s well-being. From changes in digestion and bodily functions to the emotional toll it can take, it is crucial for individuals to receive the necessary support and care to navigate these changes successfully. With the right medical and emotional support, individuals can adapt and thrive post-vagotomy, ensuring a better quality of life.
Alternatives to Vagus Nerve Cutting
Given the invasive nature of vagotomy, medical researchers are continuously exploring alternative treatments that offer similar benefits without resorting to surgical interventions. Here are two noteworthy alternatives:
Non-Invasive Vagus Nerve Stimulation
Through the use of electrical impulses, non-invasive vagus nerve stimulation (nVNS) has emerged as a promising alternative. This therapy involves the application of a small device to the neck, which delivers targeted stimulation to the vagus nerve. By stimulating the vagus nerve, nVNS aims to activate the body’s natural healing mechanisms and promote overall well-being.
Studies have shown that nVNS can have a positive impact on various conditions, including migraines, depression, and epilepsy. The electrical impulses delivered by the device help regulate the activity of the vagus nerve, which in turn influences the functioning of different organs and systems in the body.
One of the significant advantages of nVNS is its non-invasive nature. Unlike vagotomy, which requires surgery and carries risks of complications, nVNS can be administered without any incisions or anesthesia. This makes it a safer and more accessible option for individuals who may not be suitable candidates for surgery.
Furthermore, nVNS can be easily self-administered at home, under the guidance of a healthcare professional. The device used for nVNS is small and portable, allowing individuals to incorporate the therapy into their daily routines. This convenience and flexibility make nVNS a convenient alternative for long-term management of conditions that may require vagotomy.
Lifestyle Changes and Natural Therapies
Adopting a holistic approach to managing conditions that may require vagotomy is invaluable. While medical interventions are often necessary, lifestyle modifications and natural therapies can play a crucial role in improving overall well-being and reducing the need for invasive procedures.
Regular exercise is one lifestyle change that can have a significant impact on the health of the vagus nerve. Physical activity helps increase blood flow and oxygenation, which promotes the optimal functioning of the nervous system. Engaging in activities such as walking, swimming, or yoga can help stimulate the vagus nerve and enhance its effectiveness.
In addition to exercise, maintaining a balanced diet is essential for supporting vagus nerve health. Consuming foods rich in omega-3 fatty acids, such as fatty fish, walnuts, and flaxseeds, can help reduce inflammation and support nerve function. Incorporating fruits, vegetables, and whole grains into the diet provides essential vitamins and minerals that contribute to overall nerve health.
Stress reduction techniques, such as meditation and deep breathing exercises, can also have a positive impact on the vagus nerve. Chronic stress can impair vagus nerve function, leading to various health issues. By practicing relaxation techniques, individuals can activate the body’s relaxation response, which helps restore the balance of the autonomic nervous system.
Furthermore, natural therapies like acupuncture and herbal remedies may complement traditional treatment approaches. Acupuncture, a practice rooted in traditional Chinese medicine, involves the insertion of thin needles into specific points on the body. This technique is believed to stimulate the flow of energy and restore balance within the body, including the vagus nerve.
Herbal remedies, such as chamomile tea or lavender essential oil, are known for their calming properties and can help reduce stress and anxiety. However, it is crucial to consult with a healthcare professional before incorporating any natural therapies into a treatment plan, as they may interact with medications or have contraindications.
In conclusion, while vagotomy may be necessary in certain cases, exploring alternatives such as non-invasive vagus nerve stimulation and adopting lifestyle changes and natural therapies can provide additional options for individuals seeking to manage conditions without resorting to surgical interventions. These alternatives offer the potential for similar therapeutic effects with fewer risks and complications, providing hope for a more holistic approach to healthcare.
The Future of Vagus Nerve Treatments
The medical field is constantly evolving, and there is ongoing research and development in the realm of vagus nerve treatments. These advancements hold promise for individuals who may benefit from alternative interventions or refined surgical techniques.
Ongoing Research and Developments
Scientists and medical researchers continue to delve into the intricate workings of the vagus nerve and its potential applications in various conditions. Ongoing studies aim to further refine approaches like nVNS, discover new therapeutic uses, and improve our understanding of the complex interplay between the vagus nerve and the human body.
Emerging Trends in Neurology
Neurology, as a field, is witnessing remarkable progress, and the vagus nerve holds significant potential. From exploring innovative applications in managing chronic pain to addressing neurological disorders, such as Parkinson’s disease, the future of vagus nerve treatments looks promising.
In Conclusion
The decision to cut the vagus nerve is not one that is taken lightly. It is a complex procedure that is usually considered as a last resort when other treatment options have been exhausted. Individuals facing such decisions should have thorough discussions with qualified medical professionals who can provide an accurate and personalized assessment of the risks and benefits. As medical research continues to advance and new alternatives emerge, the future of vagus nerve treatments holds hope for improved outcomes and quality of life.